
The small intestine is the powerhouse of the digestive system, accounting for 90% of the digestion and absorption of the food we eat, and is also the largest part of the gastrointestinal (GI) tract at an average of 20 feet long. The inside of the small intestine is made of finger-like protrusions called villi, which, in combination with overall length, give the small intestine 2,700 square feet of absorptive area! That’s the size of a tennis court. In my opinion, the intestines were misnamed since the “large” intestine only received this name due to it being a little bit bigger in diameter (4-6cm) than the “small” intestine (3.4-4.5cm).
As the powerhouse of digestion, the small intestine must handle many things that come through it, like gastric secretions, enzymes, food particles, bacteria and other pathogens. The small intestine regulates which particles stay in, and which go out, via diffusion, into the blood stream. This regulatory process is more complicated than originally thought and has been the basis for many new health-related discoveries. Though much has been discovered, much mystery remains as to the exact mechanisms involved.
The Gate Keeper
In the walls of the small intestines are spaces between the cells that are usually closed. These spaces are called Tight Junctions and are the mechanism by which selected small molecules (amino acids, electrolytes, water and other nutrients) are allowed into the bloodstream to be used by the body. Tight Junctions are like gates that open and close and the gate keeper is a protein called zonulin. As of now, zonulin has been the only identified mediator that regulates our intestinal permeability, or the opening and closing of the gates. Various things increase the release of zonulin which, then determines the amount the tight Junctions are open and for how long they remain open.

Malfunction Junction
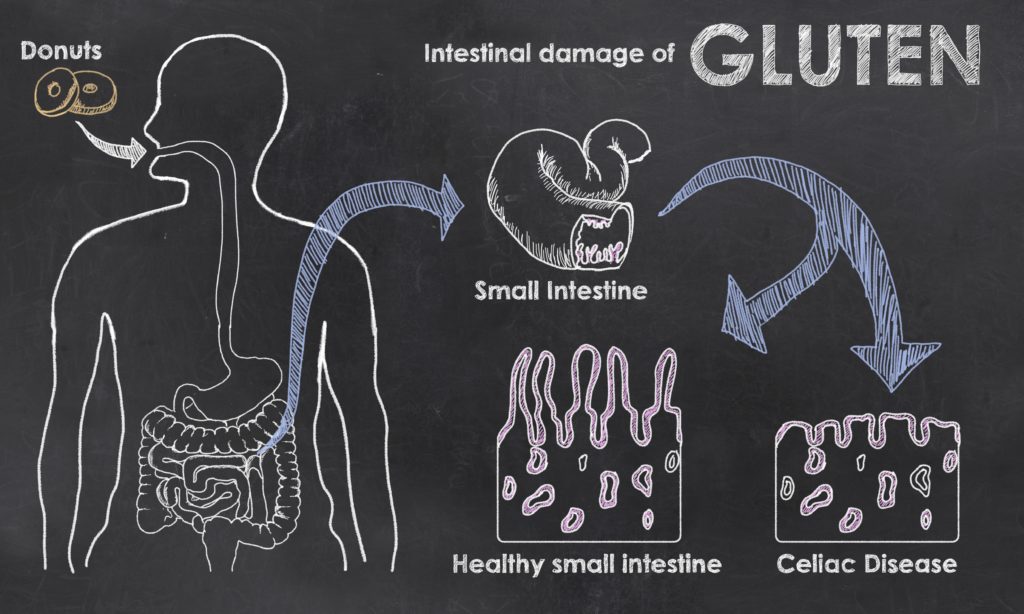
Normally, the small intestine works beautifully to bring only nutrients from fully digested foods to the body, all the while protecting the body from undigested food particles, bacteria and toxins. Some individuals are genetically predisposed to having tight junctions malfunction. In these individuals, zonulin is upregulated or “overreacts” to stimulus causing tight junctions to open at the wrong time or remain open for too long. These individuals are at a higher risk for developing Celiac Disease, because the gluten protein is much more likely to go through the intestinal lining via malfunctioning tight junctions. The immune system will then react by attacking the gluten protein. With continued exposure to gluten, the immune system can get confused and begin to attack the gastrointestinal tract.
Most often, this genetic variation does not cause any issues until an environmental factor is also involved. Unfortunately, the number of environmental factors, that stress our small intestine, have greatly increased, to the point that we are seeing increased incidence of Celiac Disease. Furthermore, we are even seeing people, without this genetic predisposition, developing issues with tight junctions in the small intestine. This malfunction is called increased luminal permeability or “leaky gut syndrome” and is being linked to many health conditions on the rise today.
What Does Leaky Gut, Unchecked, Lead To?
As mentioned in the previous section, when things that don’t belong, “leak” through the small intestine, the immune system will react to the foreign invaders. Individuals may not notice, for some time, that anything is awry. Overtime and left unchecked, leaky gut syndrome can lead to food sensitivities, chronic inflammation and autoimmune diseases like Crohn’s and Ulcerative colitis (the immune system attacking the gut), Multiple sclerosis and Parkinson’s (the immune system attacking the brain and nervous system), type 1 diabetes (immune system stacking the pancreas), Hashimotos thyroiditis (the immune system attacking the thyroid causing hypothyroidism) and so on.
Leaky gut can also cause a lot of issues with absorption of healthy nutrients, leading to deficiency and malnutrition. The most common deficiencies are iron, B12, zinc and magnesium. Deficiencies in these nutrients can lead to many different symptoms to include hair loss, severe fatigue, muscle cramps and rashes.
A Vicious Cycle
If environmental factors causing leaky gut are not removed, and the gut healed chronic inflammation will set in. This inflammation, in and of itself, perpetuates leaky gut because the white blood cells release things called mediators (histamines, prostaglandins, leukotrienes and cytokines to name a few) to attack the foreign particles leaky through. Unfortunately, these mediators left unchecked and continuously being released, cause damage to the body’s tissue, in this case, the lining of the intestine. This damage only worsens leaky gut, which then worsens inflammation which then… you get the point.
What Environmental Factors Cause Leaky Gut?
- Undiagnosed food sensitivities – this perpetuates chronic inflammation, which increases leaky gut.
- Gliadin – a component of gluten, naturally increases zonulin in everyone. For many people this doesn’t cause issues because, even though their tight junctions open, the junctions then close much more quickly than those who are genetically predisposed to malfunctioning of the tight junctions.
- Alcohol – generates nitric oxide and promotes the growth of bacteria in the intestine, that do not belong there.
- Food additives – microbial transglutaminase/TG enzyme or “meat glue”, sugars, sodium, emulsifiers (Polysorbates, cellulose/guar/zanthum gum, carrageenan, lecithin and polyglycerols), organic solvents and food dyes.
- Medications – non-steroidal anti-inflammatory (NSAIDs), vaccinations (particularly HPV and flu vaccines), antibiotics, proton-pump inhibitor (antacids)
- Stressful lifestyle left unchecked – due to chronically elevated levels of cortisol
- Systemic inflammation – the vicious cycle mentioned above
- Parasitic, bacterial or viral infections
- Radiation and Chemotherapy
Health Conditions Associated with Leaky Gut
- Celiac Disease
- Type 1 diabetes
- Crohn’s disease
- Other autoimmune diseases: ankylosing spondylitis, multiple sclerosis, rheumatoid arthritis, lupus, Hashimotos Thyroiditis
- Asthma
- Irritable bowel syndrome (IBS)
- Food allergies and intolerance
- Cancer – particularly brain, breast, lung, ovarian and pancreatic
- Obesity due to insulin resistance
How Do You Know If You Have Leaky Gut?
There are a few diagnostic tests available, but they are mostly used in well-controlled research labs due to difficulty in interpreting results because of so many variables that occur outside of a controlled laboratory.
The symptoms below are a good indicator but it is best to meet with a healthcare professional who can help guide you.
- Chronic diarrhea, constipation, gas or bloating (usually labeled as IBS)
- Fibromyalgia
- Vitamin and mineral deficiencies
- Poor immune system
- Headaches, migraines, brain fog, memory loss
- Excessive fatigue
- Skin rashes and problems such as acne, eczema or rosacea
- Cravings for sugar or carbs
- Arthritis or join pain
- Depression, anxiety, ADD, ADHD
- Autoimmune diseases
- Food sensitivities
How to Heal
- Eliminate processed foods and turn to whole foods. This will involve more cooking from scratch and meal prep. We should all do this.
- See a healthcare professional (yours truly) to see if you have a food sensitivity. If you do not eliminate foods causing inflammation your gut cannot heal (remember the vicious cycle). Eventually, under the care of said healthcare practitioner, you may be able to incorporate foods back into your diet.
- Find alternatives to NSAIDs and antacids


- Stress management, stress management, stress management!
- Some supplements that may help (again, it is best to start these with the guidance of a professional)
- Digestive enzymes
- Betaine hydrochloric acid (HCL)
- Fiber
- Collagen
- L-Glutamine
- Probiotics
- Zinc and B12
References
- Balda M. Fallon M, Van Italie C, Anderson J. Structure, regulation and pathophysiology of tight junction in the gastrointestinal tract. Yale Journal of Biology and Medicine. 1992; 65(6): 725-740
- Fasano A. Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer. Physiol Rev. 2011; 91(1): 151-175
- Stewart E. Leaky gut syndrome – Learn about the causes associated conditions and treatments under research. Today’s Dietitian. 2016 18(1): 46
- Lionetti E, Catassi C. The role of environmental factors in the development of celiac disease: what is new? Diseases. 2015 3: 282-283.
- Torsten M, Aaron L. Microbial transglutaminase is immunogenic and potentially pathogenic in pediatric celiac disease. Front Pediatr. 2019.
- Fasano A. Intestinal zonulin: open sesame! Gut. 2001; 49: 159-162
- Sapone A, Lammers K, Casolaro V, Cammarota M, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Medicine. 2011; 9:23.



